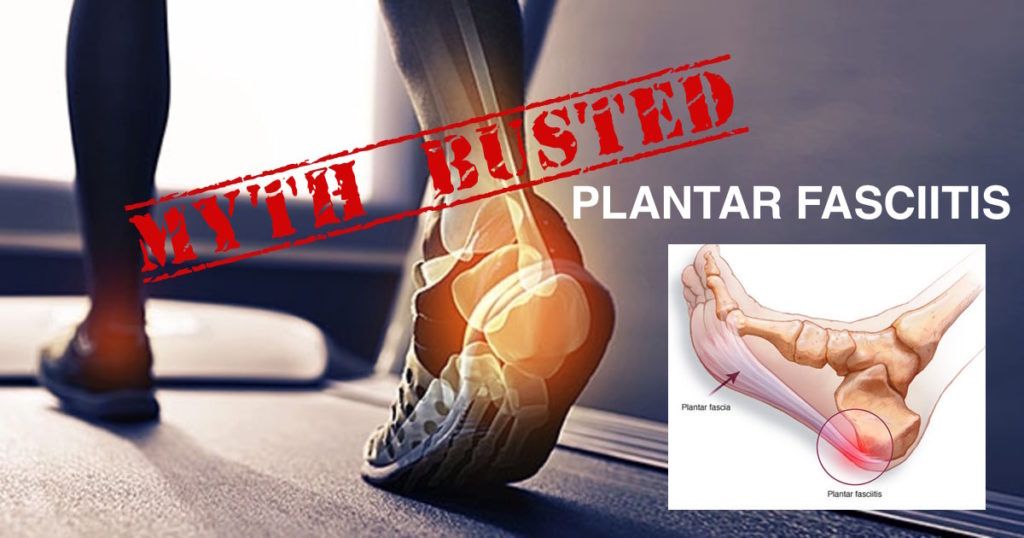
Plantar Fasciitis Treatment – Myths Exposed
Plantar fasciitis is a very common condition resulting in chronic heel pain. The condition represents irritation / inflammation of the plantar fascia. With progression, tears in the plantar fascia may develop. The pain is classically worse in the mornings or following long periods of rest.
Given how common plantar fasciitis is, many myths have arisen surrounding this condition and plantar fasciitis treatment. Dr. Mike Smith discusses some of the more common misconceptions.
Plantar Fasciitis represents a torn ‘foot muscle’
While there are many small muscles in the foot, the plantar fascia is not one of them. The plantar fascia is a thick broad fibrous band that supports the arch of the foot. It runs from the calcaneus (heel bone) to the toes, and has an important function during weight bearing and ambulation. The plantar fascia actually runs superficially over the top of the small muscles of the sole of the foot. Repetitive stretching or ‘tearing’ of the plantar fascia can cause localised irritation and pain under the heel. Without appropriate treatment, plantar fasciitis can become a chronic debilitating condition.
Plantar Fasciitis is cause by heel spurs
A very common misconception is that plantar fasciitis is caused by heel spurs. This is an understandable assumption, given that many patients with plantar fasciitis also have a heel ‘spur’. A ‘heel’ spur is seen in up to 10% of the normal population and represents a bony outgrowth from the under surface of the heel bone (calcaneus). This finding is often diagnosis on plain x-rays of the foot.

Fortunately there is no direct link between plantar fasciitis and the presence of heel spurs, and many people with heel spurs have no pain at all in their feet. Plantar fasciitis treatment does not require the removal of this spur, which would require a larger ‘open’ surgical approach.
Plantar fasciitis is hereditary
Many medical conditions have now been found to have a genetic predisposition. Other common foot conditions, such as bunion formation, also falls into this category. Plantar fasciitis however, does not have any known genetic predisposition. i.e Just because your mum has it, doesn’t mean that you will get it! While plantar fasciitis can occur in any age group, it is most frequently seen between the ages of 40 to 60.
Plantar fasciitis only occurs in those with ‘flat feet’
Up to 10-20% of the population are thought to have ‘flat feet’. But what does this mean? Having flat feet relates to collapse of the arch of the foot resulting in the entire (or close to) sole of the foot making contact with the ground when standing. This posturing can place increased strain on the plantar fascia. However, plantar fasciitis can also be seen in patients with ‘normal’ foot arches, and even in patients with ‘high arched’ feet. So even if you don’t have flat feet, your heel pain may still be caused by plantar fasciitis.
There is no ‘cure’ for plantar fasciitis
Like most conditions in medicine, it is very important that a ‘blanket’ treatment plan is not applied to everyone. Every patient has a unique constellation of symptoms and severity of the condition. While Plantar fasciitis is the most common cause of heel pain, there are several other causes that need to be excluded. These include a stress fracture of the calcaneus, nerve irritation, achilles tendonitis, and arthritis. Dr. Smith will perform a detailed assessment of your condition and construct a tailored management plan to help get you back on your feet!
Plantar fasciitis Surgery is a ‘big’ operation
Traditional ‘open’ plantar fasciitis surgery required a lengthy incision along the inner sole of the foot. The plantar fascia was released, and any bone spur was removed. Thankfully, this is no longer required.
With the use of more advanced techniques, and an understanding that the ‘heel spur’ is not a contributing factor, a plantar fasciitis release can be performed through 2 tiny keyhole incisions. This technique minimises scarring and allows for a quicker recovery. This procedure is performed as a day case, and immediate weight bearing is encouraged. Dr. Smith performs this procedure.
