Relevant Anatomy
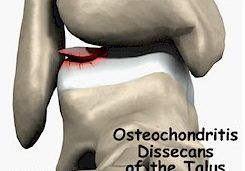
The ankle joint itself is made up of the two bones in the lower leg (tibia and fibula) and the talus (large bone that connects to both the tibia and fibula). The talus is a unique dome shaped bone. No muscles attach to the talus, and it has the highest percentage of articular cartilage coverage of any bone in the body, approximately 60% of its surface area.

Articular cartilage is a smooth white tissue that covers the end of bones that ‘articulate’ together to form joints. This cartilage is also called hyaline cartilage and is largely formed from Type 2 collagen.
When ankle cartilage damage occurs, this commonly affects the ‘articular’ cartilage of the talus.
Common Location of Ankle Cartilage Damage
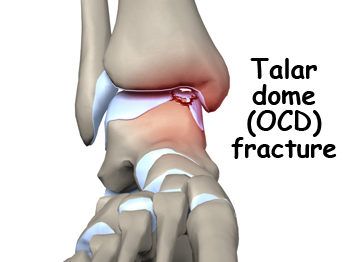
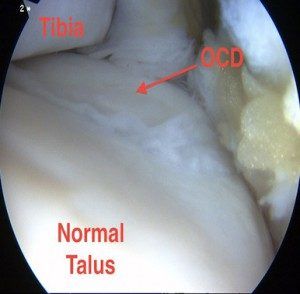
Localised ankle cartilage damage is frequently seen in two regions of the talus. This lesion is termed an osteochondral defect (OCD). The two most common locations are:
 Anterolateral Talar OCD
Anterolateral Talar OCD
This lesion is located in the outer front area of the talus dome. This usually occurs due to an inversion and dorsiflexion injury where this region of the talus cartilage ‘impacts’ against the fibula, resulting in the damaged cartilage.
 Posteromedial Talar OCD
Posteromedial Talar OCD
This lesion is located in the inner back area of the talus. While this represents a more common location for an OCD, the association with an injury is less consistent.
Ankle cartilage damage – Clinical features
Clinical features of localised ankle cartilage damage (Talus OCD) are dependent on the location and severity of the ‘lesion’. Classically patients experience pain, swelling, locking, and swelling of the ankle joint.
Anterolateral Talar OCD
These lesions are more likely to be secondary to an acute twisting injury of the ankle. They can frequently be missed on plain xrays, given the subtle appearance.
Patients often experience ongoing pain over the outer (lateral) aspect of the ankle joint, with a persistent ‘catching’ sensation and swelling. Difficulty with activities, and walking on uneven ground is also experienced.
Posteromedial Talar OCD
These lesions are more common than the ‘Anterolateral’ location. A discrete injury has not always occurred. Pain on the inside (medial) of the ankle joint, with catching and clicking, and swelling can be experienced.
Making the Diagnosis and Staging the Lesion
While the diagnosis may sometimes be clear, it can also be difficult in more subtle cases. Dr. Smith will take a thorough history of any precceding symptoms or injury that you may have sustained. An examination for localised areas of tenderness and swelling is assessed.
Plan weight bearing xrays may show signs of the damaged ankle cartilage (OCD).

A CT scan or MRI scan is ordered to help ‘stage’ the severity of the lesion, and look at the integrity of the surrounding anatomy.
There are 4 main stages to the condition and each requires different treatment.
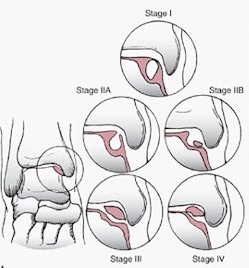
Stage 1
Articular cartilage is intact. May be presence of subchondral (below the joint) compression fracture.
Stage 2
Lesion is partially detached from its origin.
Stage 3
Lesion is completely detached but remains in the same approximate position.
Stage 4
Lesion is completely detached and has moved to another part of the ankle joint.
Treatment of localised ankle cartilage damage
The management of localised ankle cartilage damage, talar OCD, is complex.
Early stages of the condition may be managed conservatively with restriction in weight bearing and boot/cast immobilisation. If these measures fail, or in the setting of an ‘unstable’ lesion, then operative management is warranted.
Stage 1
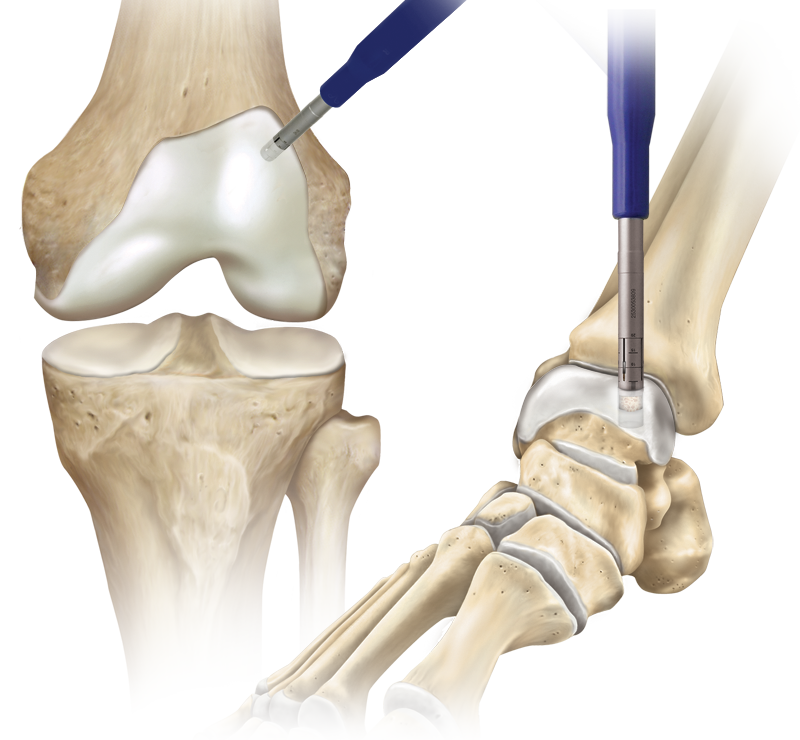
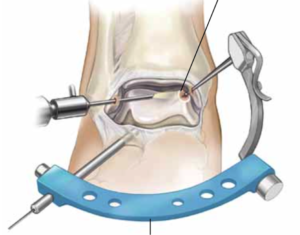
‘Drilling’ of the lesion may be performed to help stimulate blood flow to the area and healing. This can usually be done via a keyhole arthroscopy.
Stage 2
Depending on the size of the lesion at arthroscopy, a decision is made as to whether to excise the unstable fragment, versus attempt fixation with small ‘pins’.
Stage 3
Assessment of the lesion is required via an arthroscopy. All attempts are made to fixate the unstable lesion with the use of small screws/pins.

Stage 4
This is the most severe form of the condition, and it is not always possible to repair the injured cartilage. In this setting, other cartilage restoration techniques need to be considered.
Do you experience any of the following?
Frequent Ankle Sprains
Pain in your ankle
Swelling around your ankle
Learn more about Ankle Arthroscopy



