Anatomy of the achilles
The achilles tendon is the thickest tendon in the body. It is the tendon at the back of the leg that connects the calf muscles (Gastrocnemius and Soleus) to the Heel bone (Calcaneus).
This connection allows you to ‘plantar-flex’ your foot, which is used during during normal walking. Propulsion during running and jumping activities require an intact achilles tendon.

Mechanism of achilles rupture
An achilles rupture can occur spontaneously. It can also be seen in people that have had a vague pain or ‘tightness’ at the back of their calf for a period of time. In this scenario, the tendon has usually undergone a degree of degeneration prior to the ‘acute’ injury.
An achilles rupture is most frequently seen in middle aged recreational sporting enthusiasts.
The mechanism of injury is usually either :
- During a forceful ‘push-off’ with your foot, when taking off to run.
- If you trip over and you put your foot out to brace your fall – resulting in an over -stretching of the tendon

Achilles rupture – making the diagnosis
Patients who experience an achilles rupture typically describe hearing a loud ‘snap’ with immediate pain at the back of the ankle, and falling to the ground. Often people describe the feeling of being ‘kicked’ in the back of the ankle, but when they look around, there is no one near them.
Dr. Smith will take a thorough history to elicit the mechanism of injury and determine if there was any preceding symptoms.
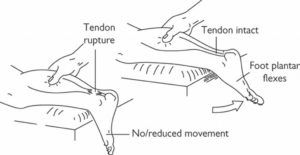
A physical examination will reveal a palpable defect in the tendon, at the site of the tear, with localised tenderness. Weakness in ankle ‘plantar flexion’ is also present.
While the diagnosis is often made based on a clinical history and examination alone, often an ultrasound or MRI scan is performed to confirm the ‘level’ of the injury, and any associated degeneration within the tendon.
Treatment of achilles rupture
All Achilles tendon ruptures should be managed actively. An early diagnosis and management plan is required for optimal outcome.
Depending on the age of the patient, level of function, and other comorbidities, a decision between nonoperative management and surgical repair of the tendon is made.
This involves the use of a CAM boot and protected weight bearing with crutches. The addition of ‘heel wedges’ are used to help approximate the tendon ends whilst healing occurs.
The CAM boot is typically required for 10 weeks, with gradual removal of the ‘heel wedges’ over time.
Surgical repair of the achilles tendon allows a direct ‘end to end’ repair of the torn tendon. This technique reduces the risk of sustaining a repeat rupture of the tendon, and maximises future ‘push-off’ strength of the calf muscles.


What is achilles tendinitis?
Achilles tendinitis / tendonitis actually refers to inflammation of the achilles tendon. This is a commonly used term amongst the general public, however we now know that the source of pain in this condition, is secondary to tendon degeneration, rather than ‘inflammation’.
What is achilles tendinosis?
In contrast to achilles tendinitis, the term achilles tendinosis refers to the achilles tendon undergoing degeneration over time, leading to this chronic condition.
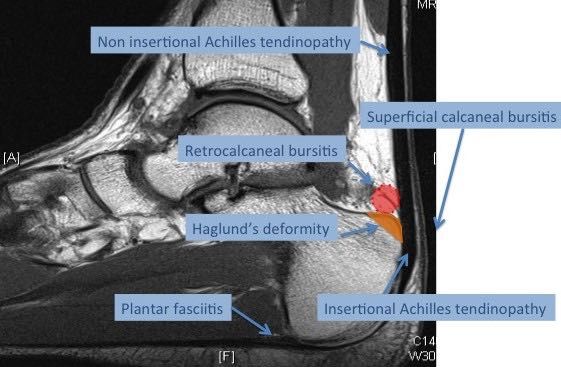
Achilles tendinosis can classically occur in two distinct areas of the achilles tendon
Non-Insertional Achilles Tendinosis
This condition results in degeneration of the middle area (mid-substance) of the achilles tendon. This is typically seen in younger active people and can be very debilitating.
Insertional achilles Tendinosis
This condition relates to degeneration of the tendon as it inserts into the heel bone (calcaneus). It may be present in association with a bony bump (Haglund deformity) at the back of the heel and bursitis.
Insertional tendinosis can be a very difficult condition to manage and requires a thorough assessment.
Clinical presentation of achilles tendinitis/ tendinosis
Patients typically present with chronic (long-term) pain at the back of the heel, which is often exacerbated by exercise. A feeling of ‘tightness’ of the calf muscles is usually present, and patients often notice a ‘bump’ or enlargement of the tendon. Difficulty with shoes rubbing is common.
Achilles tendinitis / tendinosis – Making the diagnosis
The diagnosis is often clear based on the history and examination findings.
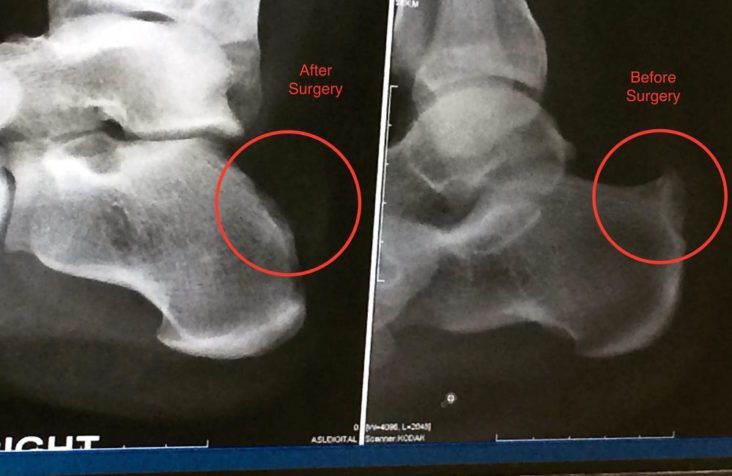
A plain x-ray assesses the degree of bony protuberance that is present, and any additional pathology such as arthritis is looked for.

An MRI scan is the best imaging modality to assess the integrity of the achilles tendon itself. The location and severity of the degeneration is seen.
Treatment of Achilles tendinosis
Achilles tendinosis is best managed with an active management plan, following a thorough assessment.
An initial period of ‘rest’, anti-inflammatories, and achilles stretching, is followed by a structured strengthening program.
If the symptoms fail to settle, surgical debridement of the degenerative tendon and removal of any excess bony protuberance or bursitis (inflamed tissue) is performed.
Do you experience any of the following?
Pain over your achilles tendon
Tightness of your calf muscles
A bony prominence at the back of your heel

